Advance Care Planning and End of Life Care
In the previous blog I wrote about Making my Advance Decision to Refuse Treatment and commented on specific Advance Care Planning for a person approaching the end of life; here I follow up and explore what Advance Care Planning at the end of life might look like.
What does End of Life Care Mean?
Contrary to popular belief, end of life care (EoLC) is not about dying; planning for last days of life is part of end of life care but by no means the whole story. You might also hear the term Palliative and End of Life Care (PEoLC) - terminology in end of life care warrants another another blog another time.
The NHS provides the following definition of end of life care:
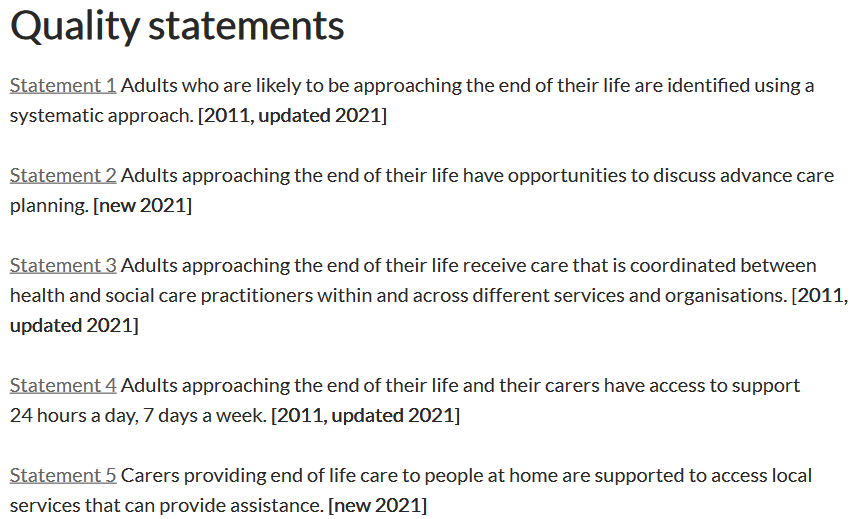
National guidance provides a clear framework of what end of life care should include:
You’ll notice Advance Care Planning is one of the key statements.
Looking specifically through an end of life care lens, the next sections will consider what Advance Care Planning might look like in three stages; firstly, from diagnosis of a long-term condition, secondly, when a person may be in the last months of life and, in the third section, Advance Care Planning in the last days of life.
Advance Care Planning with a long-term condition
Good Advance Care Planning with a long-term condition is about zooming out, it’s about looking at the big picture of the illness and checking in to see what might happen next and what would be most important to you. It’s not meant to dominate all conversations or thoughts, but it is about being aware how the illness you have may changes over time and where you are in that story of change.
Specific Advance Care Planning could include making sure you have Lasting Power of Attorney in place or creating an Advance Decision to Refuse Treatment. It’s important to consider that a Lasting Power of Attorney takes around twenty weeks to register, so it’s not something you can leave until you need it. A recent Which? poll found there was a mistaken belief that LPAs could be set up as needed finding “77% (of people) thought it could be set up whenever”. The article continued to present another finding of the poll with 70% of those polled saying “they were healthy so did not need one.” You can read more about this in the blog Changing Fears to Facts .
Other elements of Advance Care Planning at this stage could include making or updating your will and Digital Legacy, and confirming your choices regarding Organ Donation. Over the years in PEoLC I have heard countless times of people who wish to donate their body Medical Education but often this has been left too late, something I explore in Donating Your Body for Medical Education with Kim Claridge and with my Aunt who is specifically donating her brain for Parkinson's Disease research.
Having a conversation about wishes around cardiopulmonary resuscitation (CPR) is often introduced to establish wishes and preferences around CPR. There is a great Planning Ahead Tool from Hospice UK which explains different scenarios in which CPR may be considered; as a treatment when a heart stops unexpectedly, when CPR is unlikely to succeed and when CPR is not desirable.
Starting an Advance Care Plan to document your wishes is a good idea at this stage and your palliative care team or hospice should be able to direct you to any locally used forms. It’s also an opportunity to consider Memory Making.
In summary, planning ahead when diagnosed with a long-term condition could include:
· Lasting Power of Attorney
· Advance Decision to Refuse Treatment
· Local Advance Care Plan
· Organ Donation
· Donating your body for medical education
· Exploring views around cardiopulmonary resuscitation.
· Digital Legacy
· Memory Making
· Will
Advance Care Planning in last months of life
Moving now to think about what Advance Care Planning could look like when life may be measured in months. All of the above still apply, however, there will be additional considerations.
In the last months of life a person is eligible for continuing healthcare fast-track funding, for immediate provision of NHS continuing healthcare.
It would also be appropriate to re visit CPR decisions as some conditions will make CPR very unlikely to succeed. A Do Not Attempt Cardio Pulmonary Resuscitation (DNACPR) for can be used to protect you from a medical treatment that may no longer be appropriate. In some areas a ReSPECT process or form is used which includes plan for emergency situations, in other areas this is a separate form and might be know as a Treatment Escalation Plan (TEP). Whatever the title, a good TEP or ReSPECT document will include clear management plans for different situations that could occur, and what your wishes would be.
An overarching document which would help bring your wishes together in the last months of life is an Advance Care Plan. For a person in the last months of life it is a good idea to source and complete a local Advance Care Plan with support of your palliative care team, community team or GP. For a person wishing to die at home, Advance Care Planning might include equipment such as a hospital bed or mattress to prevent skin damage.
In summary, planning ahead in last months of life could include:
· Fast Track Continuing Health Care
· DNACPR (ReSPECT)
· Treatment Escalation Plan (included in a ReSPECT)
· Completing a local Advance Care Plan
· Ordering appropriate equipment of a person wishes to die at home
Advance Care Planning in last days of life
Towards the very last days of life Advance Care Planning brings together the plans that have been made already, these plans are revisited and updated rather than suddenly started.
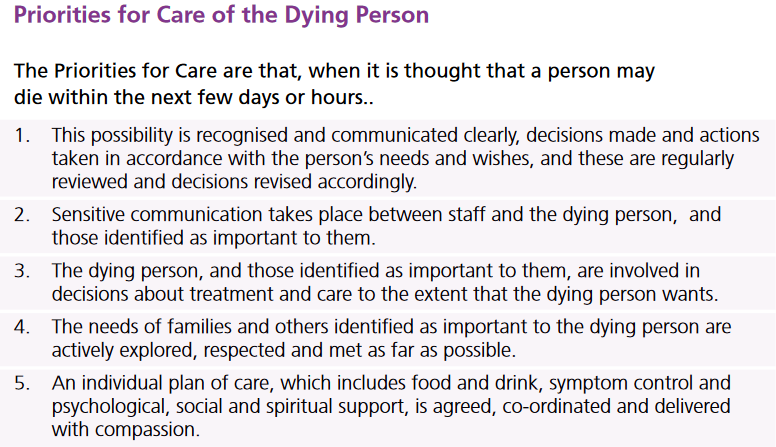
There will be some planning that is specifically considered in the last days of life; for example, the provision of medications for a “just in case” situation and a care plan for the last days of life. Having medications in place for a person who has been used to taking medications by mouth is important as there may come a time when the oral route is not possible, and the Priorities for Care of the Dying Person is used nationally as a framework for care of a dying person.
In summary, planning ahead for last days of life could include:
· Just in case medications
· A Care Plan for the Last Days of Life
· Explaining the process of Ordinary Dying
Setting out the stages of Advance Care Planning and aligning them to stages through life is a useful approach, it supports a proactive approach to planning ahead rather than a crisis response approach. The ideas above are by no means exhaustive and there is overlap between them all, there will also be plans for highly specific events which may also need consideration but the sections make a good starting place.
If you would like to learn more about how I can support you in Proactive Advance Care planning contact me