Living and working with a terminal illness: what do we know and what could we do better?
This blog is a pleasure to write, it is a chance to step back and honour where the question came from, identify what has been learned and share next steps. In the blog I’ll start with the person who contributed to the vision, describe the formal project that evolved and share the translation of the project into planning and actions.
How the question started
The question started with a remarkable lady, Clair Fisher. Clair was diagnosed with stage 4 bowel cancer whilst working abroad, a sudden and unexpected diagnosis which Clair transformed into what she called her “retirement project.”
Clair Fisher
Clair was a public policy professional with expertise in well-being, she used her knowledge and experience to campaign for three key area during her retirement project:
· Early intervention palliative care
· The benefits of working during a terminal illness
· Breaking down the taboos about death and dying
It was my privilege to link up with Clair through Twitter. We connected, shared discussions and Clair introduced me to the What Works Centre for Wellbeing an independent collaborating centre that develops and shares robust and accessible wellbeing evidence to improve decision-making.
In May 2021 it was a privilege to work with Clair and the What Works Centre for Wellbeing Dying Well: Wellbeing at the end of life. A summary of practitioner conversations .The conversations included practitioners, academics and individuals exploring what really matters to people with life limiting illness and how to develop appropriate support. Continuing to work was an area identified as important to enhance wellbeing when living with a life limiting illness.
Clair’s condition deteriorated throughout 2021, however she remained passionate about sharing her experience and raising awareness about the issues so important to her. Towards the end of her life, in December 2021, Clair Tweeted how hard it was for her voice to be heard despite meticulous Advance Care Planning. I heard Clair’s frustration, connected once more with Clair and was honoured to record How to ensure your plans are heard with Clair Fisher The podcast became the first in a series designed to improve professional understanding, raise public awareness and normalise Advance Care Planning. We recorded three weeks before Clair died and talked of the need for Important Conversations about Important Conversations.
Clair’s legacy continued with the What Works Centre for Wellbeing who partnered with Marie Curie to learn more about working with a terminal illness. The project, “Working with terminal illness:
what is known and what is needed”, included a scoping review of existing literature, a survey of HR professionals and a call to practice to identify examples of support available for people working while living with a terminal illness.
What was learned from the Working with terminal illness: what is known and what is needed project
The scoping review identified the very limited evidence available and the challenges people experience when working with a terminal illness. The findings also included the additional strain loss of income caused and the lack of evidence to date specifically about mental wellbeing gained by continuing to work.
From the survey of HR managers, over one third reported that they did not know how their terminally ill employees were supported. In contrast some employees offered a more flexible and holistic approach. In summary, the findings form HR decision makers revealed an “employer lottery” on the support, flexibility and adjustments offered to employees working while living with a terminal illness. Offering flexibility at work, creating a more open, inclusive and supportive culture and having sensitive communication were identified as themes that would make the biggest difference.
The report included practice examples such as applying the TUC's Dying to work charter and how existing policies could be applied flexibly to enable an individual to work from home while receiving treatment.
Recommendations from the project
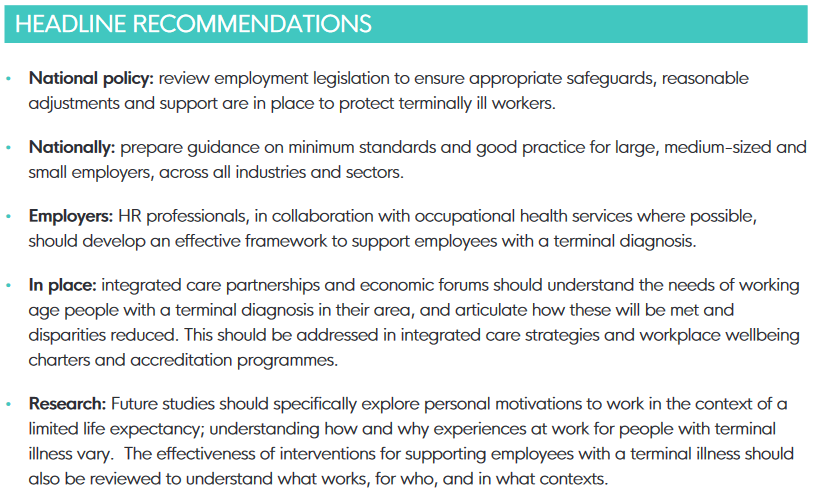
The project called for a review of national policy, working at scale and in place and development of policy and procedures within work places.
The headline recommendations are summarised below and are detailed on page 14 of the report .
You can read the full report here
I have described how the question started and the formal project, in the last section I’ll outline how the project is translating into plans and actions.
Next steps
Private Members Bill
Following publication of the report a private Member’s bill, the Terminal Illness (Support and Rights) Bill, has been raised. I was lucky to be at the Houses of Parliament Round Table discussion to hear the report presented and will be following the bill with interest.
Virtual event
The report was presented at a virtual event hosted by the What Works Centre for Wellbeing in January 2022. The event was open to researchers, occupational health and wellbeing professionals and those supporting people of working age developing work and health policy at a regional and national level.
Work place support
As a result of the virtual event described above I am delighted to have partnered with a County Council to deliver a series of workplace presentations. The presentations have been designed collaboratively in discussion with managers and representatives from the carers’ group. The pilot sessions will focus on the frameworks important to understand when supporting those with a terminal illness and identify the skills needed for sensitive communication.
General Advance Care Planning: what everyone needs to know
Lasting Power of Attorney: myth busting
How to have Conversations that Matter
Navigating the chapters of an illness: what you need to know to get the best care possible
The sessions put into action a recommendation from the report to creating an open culture, find out what could help people and encourage conversations.
The sessions will be reviewed and can be delivered and adapted to deliver nationally. Contact me to find out more if you are interested in finding out more or host a session in your work place.
Policy Guidance
Discussion is continuing to introduce formal guidance for employers supporting employees working with terminal illness. The Chartered Institute of Personnel and Development (CIPD) are developing stand alone guidance for HR on workplace support for employees with terminal illness.
Final thoughts
Setting out the beginning stages of work, reviewing the formal project and sharing the steps already being taken to make a difference to people working and living with a terminal illness has been a pleasure to write. It is fabulous to see ideas generating into research and actions develop from words.
Looking ahead; “If Dying Matters – then it matters at work too” will be a focus of the national Dying Matters awareness week 2023. This is a great opportunity to open conversations and promote a more open culture around death, dying and grief in all places – including the workplace.
To close I’m reflecting on a line from Clair’s blog written in February 2021:
“My hope is that through starting this conversation we can share existing evidence and best practice to better support those of working age who are diagnosed with a terminal illness.”
Clair, I think we can say conversations have started, evidence has been explored and let’s now start supporting people better.